Embark on a journey of nutritional discovery with PN Vital Signs Assessment 2.0, the innovative tool that transforms patient care. This comprehensive assessment empowers healthcare professionals to assess nutritional status with unparalleled accuracy, opening doors to personalized interventions that optimize patient outcomes.
Unveiling the intricacies of PN Vital Signs Assessment 2.0, this guide delves into its components, interpretation, applications, and future directions. Prepare to be enlightened as we explore the depths of nutritional assessment and its profound impact on patient well-being.
Overview of PN Vital Signs Assessment 2.0
PN Vital Signs Assessment 2.0 is an advanced tool designed to assess the nutritional status of patients, particularly those receiving parenteral nutrition (PN). It is a comprehensive evaluation that provides valuable insights into a patient’s nutritional needs and helps guide appropriate interventions.
The assessment process involves a detailed examination of various parameters, including anthropometric measurements, biochemical markers, and clinical indicators. These parameters are then analyzed in conjunction with the patient’s medical history and current condition to determine their nutritional status and identify any potential deficiencies or imbalances.
Historical Development and Implementation
PN Vital Signs Assessment 2.0 was developed based on extensive research and clinical experience in the field of nutrition support. It was first introduced in the early 2000s and has since gained widespread acceptance as a valuable tool for assessing nutritional status in PN patients.
PN vital signs assessment 2.0 is a great way to get a comprehensive overview of your health. The assessment covers everything from your blood pressure to your weight and height. It’s a quick and easy way to identify any potential health concerns.
If you’re looking for a way to get a better understanding of your health, I recommend checking out the kite fighters answer key . It’s a great resource that can help you learn more about your health and how to improve it.
Once you’ve completed the assessment, you’ll have a better understanding of your health and can make informed decisions about your health care.
Its implementation has led to significant improvements in the management of PN therapy, enabling healthcare professionals to tailor nutritional interventions to the specific needs of each patient. This has resulted in better outcomes, reduced complications, and improved overall patient well-being.
Components of PN Vital Signs Assessment 2.0
PN Vital Signs Assessment 2.0 comprises several key components, each contributing to a comprehensive assessment of a patient’s nutritional status. These components are:
- Anthropometric measurements: These include height, weight, body mass index (BMI), and waist circumference. They provide an overview of the patient’s overall body composition and nutritional status.
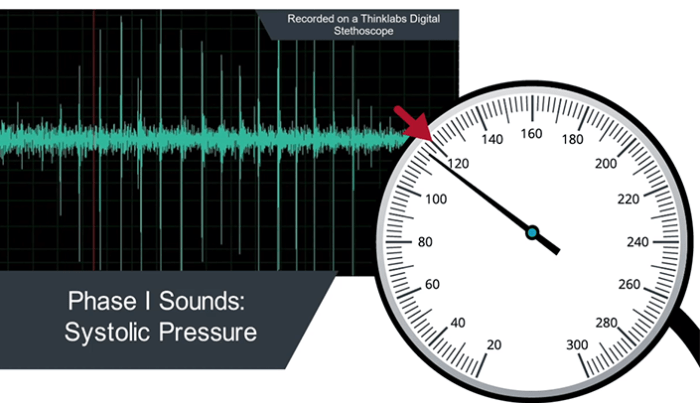
- Biochemical measurements: These include serum albumin, prealbumin, and total lymphocyte count. They assess the patient’s nutritional reserves and immune function.
- Dietary intake assessment: This involves evaluating the patient’s food and fluid intake, including calories, protein, and micronutrients. It helps determine the patient’s nutritional adequacy.
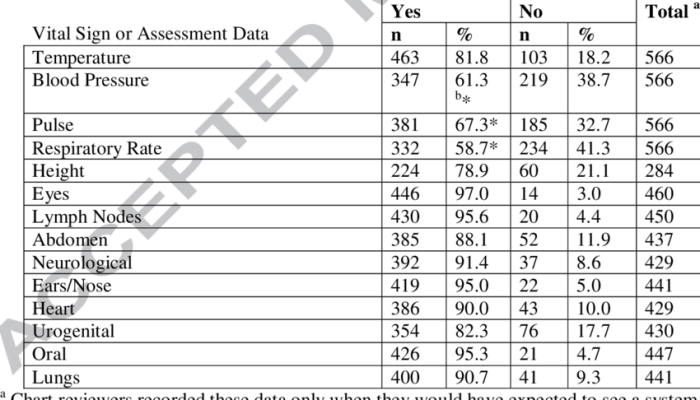
- Physical examination: This includes assessing the patient’s skin, hair, nails, and oral cavity for signs of malnutrition. It also involves examining the patient’s abdomen for any signs of ascites or organomegaly.
- Functional assessment: This evaluates the patient’s ability to perform activities of daily living, including eating, dressing, and bathing. It assesses the impact of malnutrition on the patient’s functional capacity.
By combining these components, PN Vital Signs Assessment 2.0 provides a comprehensive assessment of the patient’s nutritional status, allowing healthcare professionals to identify malnutrition early and implement appropriate interventions.
Interpretation of PN Vital Signs Assessment 2.0 Results
The PN Vital Signs Assessment 2.0 results are interpreted using a set of criteria that determine the level of nutritional risk for the patient. These criteria are based on the patient’s weight loss, body mass index (BMI), and other factors.
Scoring System
The PN Vital Signs Assessment 2.0 uses a scoring system to determine the level of nutritional risk. The score is based on the following factors:
- Weight loss
- Body mass index (BMI)
- Food intake
- Activity level
- Medical conditions
The score is used to determine the patient’s nutritional risk level, which can be low, moderate, or high.
Clinical Decision-Making
The results of the PN Vital Signs Assessment 2.0 can be used to make clinical decisions about the patient’s nutritional care. These decisions may include:
- Starting or continuing nutritional support
- Adjusting the patient’s diet
- Monitoring the patient’s nutritional status
The PN Vital Signs Assessment 2.0 is a valuable tool for assessing the nutritional risk of patients and making clinical decisions about their nutritional care.
Applications of PN Vital Signs Assessment 2.0
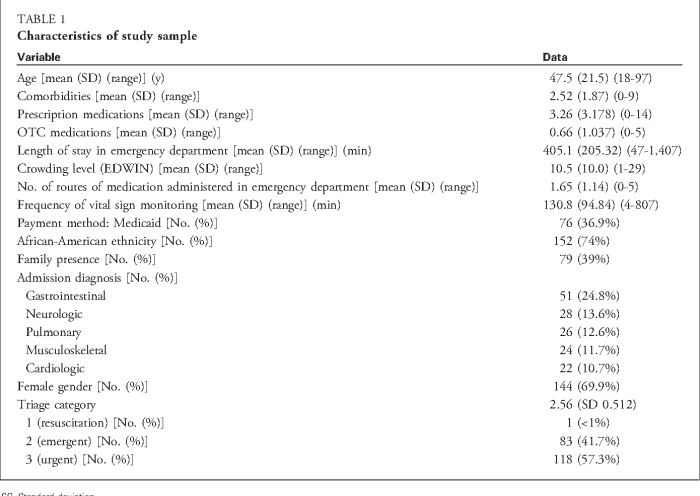
PN Vital Signs Assessment 2.0 is a comprehensive assessment tool that has been widely used in various clinical settings to evaluate the nutritional status of patients. Its applications extend across different patient populations, from healthy individuals to those with acute or chronic illnesses.
Clinical Settings, Pn vital signs assessment 2.0
- Hospital Inpatient Units:PN Vital Signs Assessment 2.0 is commonly used in inpatient settings to assess nutritional status and monitor patients’ progress. It helps identify malnutrition and provides guidance for appropriate nutritional interventions.
- Outpatient Clinics:In outpatient settings, the assessment is used to screen for malnutrition and provide nutritional counseling to individuals at risk. It aids in early detection and prevention of malnutrition-related complications.
- Long-Term Care Facilities:PN Vital Signs Assessment 2.0 is valuable in long-term care facilities, where malnutrition is prevalent among elderly residents. It assists in monitoring nutritional status and developing personalized care plans.
- Community Health Programs:The assessment is employed in community health programs to assess nutritional status and identify individuals in need of nutritional support. It helps target interventions and improve nutritional outcomes at the community level.
Patient Populations
PN Vital Signs Assessment 2.0 is applicable to a diverse range of patient populations, including:
- Critically Ill Patients:The assessment helps identify malnutrition in critically ill patients, who are at high risk due to increased metabolic demands and reduced nutrient intake. Early detection and intervention can improve patient outcomes.
- Surgical Patients:Pre- and post-operative nutritional assessment using PN Vital Signs Assessment 2.0 optimizes surgical outcomes by identifying malnutrition and providing appropriate nutritional support.
- Oncology Patients:Malnutrition is common in cancer patients due to disease-related factors and treatment side effects. PN Vital Signs Assessment 2.0 helps monitor nutritional status and guide nutritional interventions to improve tolerance to treatment and overall outcomes.
- Geriatric Patients:The assessment is crucial for geriatric patients, who often experience age-related changes in nutritional needs and are at risk of malnutrition. It assists in identifying and addressing nutritional deficiencies.
Case Studies
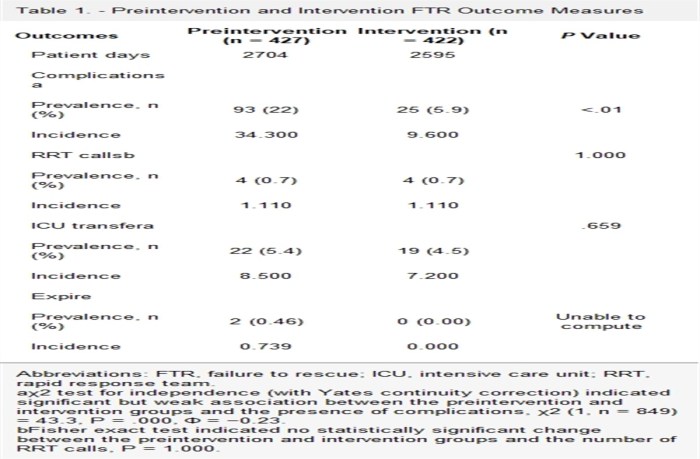
Numerous case studies have demonstrated the effectiveness of PN Vital Signs Assessment 2.0 in improving patient outcomes:
- A study in critically ill patients showed that early identification of malnutrition using PN Vital Signs Assessment 2.0 led to a significant reduction in mortality rates.
- In a study of surgical patients, pre-operative nutritional assessment using the tool helped reduce post-operative complications and shorten hospital stays.
- In geriatric patients, PN Vital Signs Assessment 2.0 facilitated early detection of malnutrition and implementation of nutritional interventions, resulting in improved functional status and quality of life.
Limitations and Considerations
PN Vital Signs Assessment 2.0 has certain limitations that users should be aware of. These limitations can affect the accuracy and reliability of the assessment results, so it is important to understand them and take steps to address them.
Factors Affecting Accuracy
- Subjective nature of the assessment:The assessment relies on subjective observations and interpretations of the patient’s vital signs and other indicators. This can lead to variations in the results depending on the observer’s experience and expertise.
- Patient cooperation:The patient’s cooperation is essential for an accurate assessment. If the patient is uncooperative or unable to provide reliable information, the results may be compromised.
- Environmental factors:The assessment can be affected by environmental factors such as noise, lighting, and temperature. These factors can influence the patient’s vital signs and behavior, leading to inaccurate results.
Recommendations for Addressing Limitations
To address the limitations of PN Vital Signs Assessment 2.0, the following recommendations should be considered:
- Training and standardization:Healthcare professionals should receive proper training on the assessment to ensure consistent and accurate observations.
- Objective measures:Whenever possible, objective measures such as vital sign monitors should be used to supplement subjective observations.
- Control of environmental factors:The assessment should be conducted in a controlled environment to minimize the impact of external factors.
- Patient education:Patients should be educated about the importance of their cooperation and how to provide accurate information.
- Regular review and evaluation:The assessment should be reviewed and evaluated regularly to identify any areas for improvement and ensure its validity.
Future Directions and Research: Pn Vital Signs Assessment 2.0
PN Vital Signs Assessment 2.0 continues to evolve, with ongoing research and advancements aimed at enhancing its utility and accuracy. Future directions and research in this area include:
Potential Advancements and Improvements
Exploring the potential for integrating AI and machine learning algorithms into the assessment process to improve accuracy and efficiency.
Ongoing Research
Conducting studies to validate the assessment’s reliability and validity in diverse patient populations and clinical settings.
Areas for Further Research
- Investigating the use of the assessment in predicting patient outcomes and guiding personalized care plans.
- Exploring the integration of the assessment with other clinical tools and technologies to enhance patient monitoring and management.
Essential FAQs
What is the significance of PN Vital Signs Assessment 2.0?
PN Vital Signs Assessment 2.0 empowers healthcare professionals to assess nutritional status with unparalleled accuracy, enabling personalized interventions that optimize patient outcomes.
How does PN Vital Signs Assessment 2.0 contribute to patient care?
By providing a comprehensive nutritional assessment, PN Vital Signs Assessment 2.0 guides healthcare professionals in identifying nutritional risks and developing tailored interventions to address individual patient needs.
What are the key components of PN Vital Signs Assessment 2.0?
The assessment includes components such as anthropometric measurements, biochemical parameters, dietary intake, and functional capacity, providing a holistic view of nutritional status.
How are the results of PN Vital Signs Assessment 2.0 interpreted?
Results are interpreted using established criteria to determine nutritional risk levels, guiding clinical decisions and appropriate interventions.